Abstract from AHA 2020 P472
- heartlung
- Jan 16, 2023
- 2 min read
Updated: Jan 18, 2023
– Ischaemic Pre-conditioning: A Non-invasive Intervention That Improves Maternal Endothelial Function in Women With Preeclampsia And at Risk of Preeclampsia

P472 – Ischaemic Pre-conditioning: A Non-invasive Intervention That Improves Maternal Endothelial Function in Women With Preeclampsia And at Risk of Preeclampsia
Author Block: Tamara Kubba, Univ Coll London Inst for Women’s Health, London, United Kingdom; Sean Michael Davidson, Hatter Cardiovascular Inst, UCL, London, United Kingdom; David Williams, Univ Coll London Hosp, London
Disclosure Block: T.Kubba: None. S.M.Davidson: None. D.Williams: None.
Introduction:
Preeclampsia is a pregnancy syndrome defined by the gestational onset of hypertension and proteinuria and characterised by maternal endothelial dysfunction with placental ischaemia. Preeclampsia affects approximately 4% of first-time pregnant mothers, but approximately 20% of women with pre-existing hypertension. Ischaemic pre-conditioning (IPC) is a phenomenon whereby transient episodes of ischaemia protect against future ischaemic injury. IPC has never previously been studied in pregnant women. We investigated whether IPC could improve maternal endothelial function in women at risk of preeclampsia and with preeclampsia.
Hypothesis:
We hypothesised that IPC would improve maternal endothelial function in women with preeclampsia and at risk of preeclampsia.
Methods:
We measured brachial artery flow mediated dilatation (FMD), before and after IPC in 3 groups of pregnant women between 24+0 and 36+6 weeks gestation: normotensive pregnancy (n=42), at risk of preeclampsia (n=20) and established preeclampsia (n=11). Following a baseline measure of brachial artery FMD, 3 cycles of 5-minutes of upper arm ischaemia were alternated with 5-minutes of reperfusion. Twenty-four hours later, maternal FMD was re-measured.
Results:
Women with preeclampsia had the lowest baseline FMD 4.09% +/- 0.73%: mean +/- SEM, which increased to 6.25% +/- 0.83% (p=0.0024) following IPC. Women at risk of pre-eclampsia had baseline FMD 7.57% +/- 0.82%, which increased to 8.93% +/- 0.73% (p=0.025) following IPC. Normotensive pregnant women had the highest baseline FMD (10.32% +/- 0.69%), which did not increase further following IPC (10.52% +/- 0.69%). However, normotensive pregnant women reached peak flow-mediated dilatation more quickly following IPC; 414 s +/- 2.94 s v 425 s +/- 4.22 s (p=0.0302).
Conclusions:
IPC is a non-invasive technique that we have shown improves local endothelial function in women with preeclampsia and at risk of preeclampsia. IPC merits further study as an intervention to improve systemic endothelial function and pregnancy outcomes for women with hypertensive pregnancies. View session detail
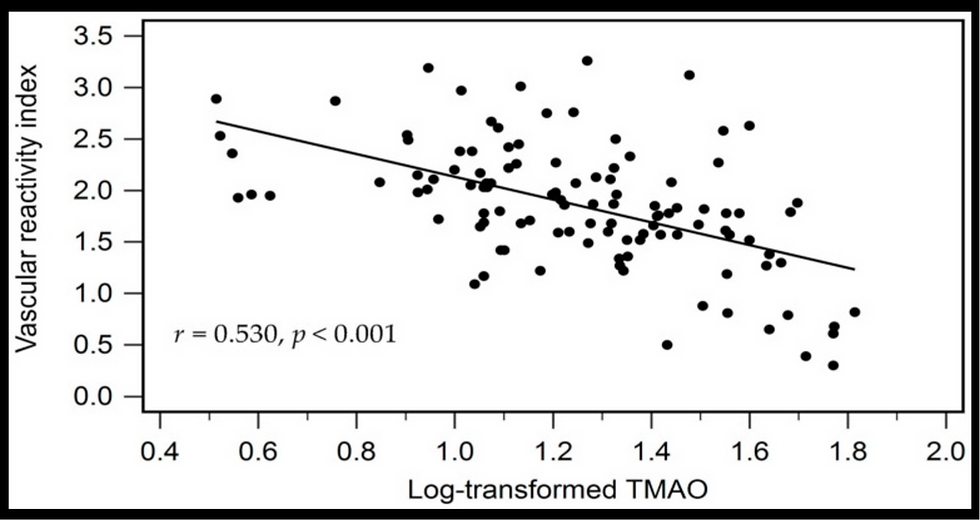
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments