Monitoring Endothelial Function while Taking Statin and PPI (proton pump inhibitor) for Two Complete
- Jan 16, 2023
- 4 min read
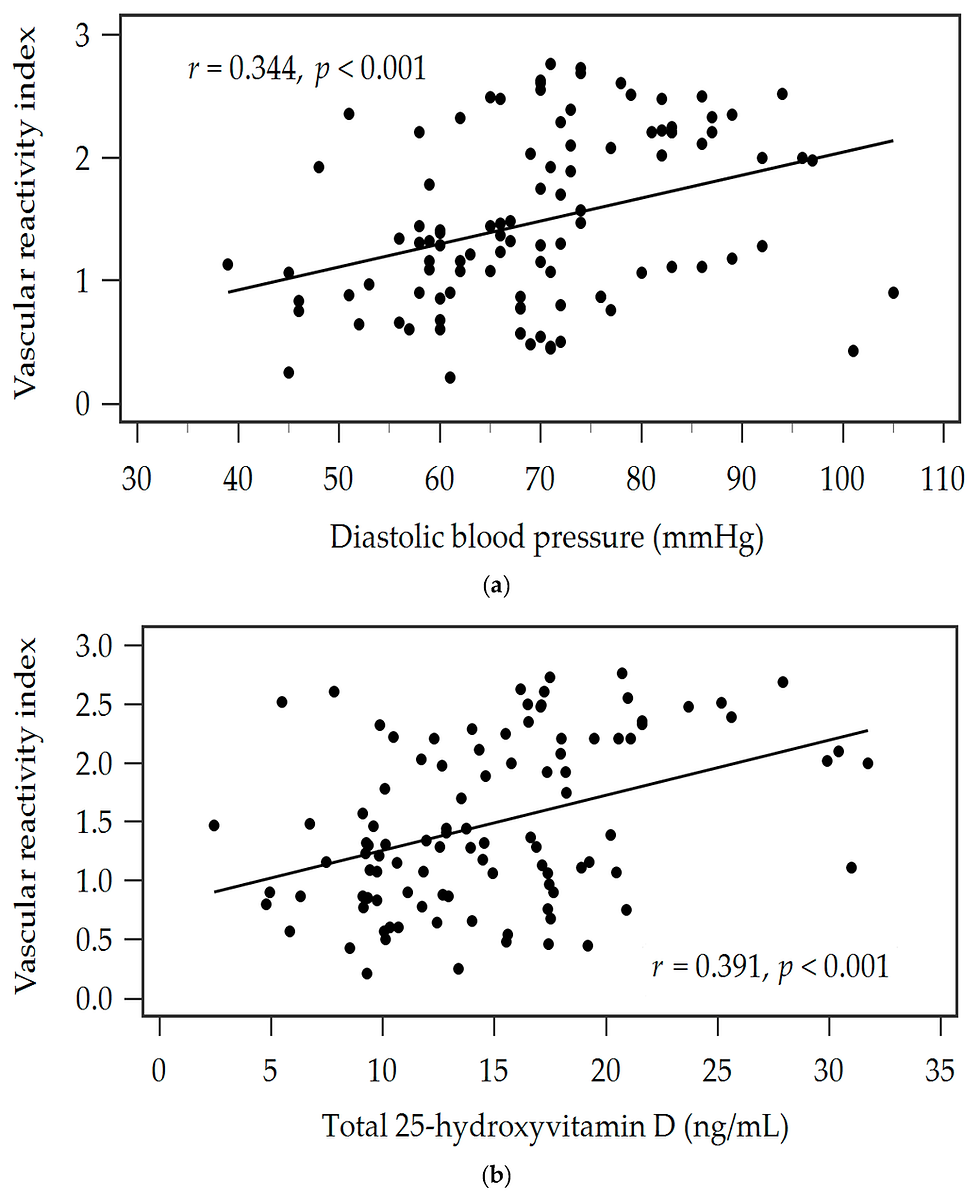
Heart Vessels. 2017 Dec 5. doi: 10.1007/s00380-017-1094-0. [Epub ahead of print] Effect of Aggressive lipid-lowering treatment with Rosuvastatin on vascular endoTHeliumfunction: evaluation of vascular endothelium function (EARTH study). Takayama T1, Hiro T2, Yoda S2, Fukamachi D2, Haruta H2, Kogo T2, Mineki T2, Murata H2, Oshima T2, Hirayama A2. Author information 1Division of Cardiology, Department of Medicine, Nihon University School of Medicine, 30-1, Ohyaguchi-kamicho, Itabashi-ku, Tokyo, 173-8610, Japan. takayama.tadateru@nihon-u.ac.jp.2Division of Cardiology, Department of Medicine, Nihon University School of Medicine, 30-1, Ohyaguchi-kamicho, Itabashi-ku, Tokyo, 173-8610, Japan. Abstract Vascular endothelial dysfunction plays an important role in the process of atherosclerosis up to the final stage of plaque rupture. Vascular endothelial dysfunction is reversible, and can be recovered by medications and life-style changes. Improvement in endothelial function may reduce cardiovascular events and improve long-term prognosis. A total of 50 patients with stable angina and dyslipidemia were enrolled, including patients who had not received prior treatment with statins and had serum LDL-C levels ≥ 100 mg/dL, and patients who had previously received statin treatment. All agreed to register regardless of their LDL-C level. Rosuvastatin was initially administered at a dose of 2.5 mg and appropriately titrated up to the maximum dose of 20 mg or until LDL-C levels lower than 80 mg/dL were achieved, for 24 weeks. Endothelial function was assessed by the reactive hyperemia peripheral arterial tonometry (RH-PAT) index in the radial artery by Endo-PAT®2000 (Endo-PAT®2000, software version 3.0.4, Itamar Medical Ltd., Caesarea, Israel). RH-PAT data were digitally analyzed online by Endo-PAT®2000 at baseline and at 24 weeks. LDL-C and MDA-LDL-C decreased from 112.6 ± 23.3 to 85.5 ± 20.2 mg/dL and from 135.1 ± 36.4 to 113.9 ± 23.5 mg/dL respectively (p < 0.0001). However, HDL-C, hs-CRP and TG did not change significantly after treatment. RH-PAT index levels significantly improved, from 1.60 ± 0.31 to 1.77 ± 0.57 (p = 0.04) after treatment, and the percent change of the RH-PAT index was 12.8 ± 36.9%. Results of multivariate analysis show that serum LDL-C levels over 24 weeks did not act as a predictor of improvement of the RH-PAT index. However, HbA1c at baseline was an independent predictor which influenced the 24-week RH-PAT index level. The RH-PAT index of patients with high HbA1c at baseline did not improve after administration of rosuvastatin but it did improve in patients with low HbA1c at baseline. Aggressive lowering of LDL-C with rosuvastatin significantly improved the RH-PAT index, suggesting that it may improve endothelial function in patients with coronary artery disease.Clinical Trial Registration No: UMIN-CTR, UMIN000010040. KEYWORDS: Endothelium function; Lipid lowering; Reactive hyperemia; Statin Curr Drug Metab. 2017 Dec 7. doi: 10.2174/1389200219666171207125351. [Epub ahead of print] Adverse events of proton pump inhibitors: potential mechanisms. Corsonello A1, Lattanzio F2, Bustacchini S2, Garasto S1, Cozza A1, Schepisi R1, Lenci F3, Luciani F4, Maggio MG5, Ticinesi A5, Butto V5, Tagliaferri S5, Corica F6. Author information 1Unit of Geriatric Pharmacoepidemiology, Research Hospital of Cosenza, Italian National Research Centre on Aging (INRCA), Cosenza. Italy.2Scientific Direction, Italian National Research Center on Aging (INRCA), Ancona. Italy.3Unit of Nephrology, Italian National Research Center on Aging (INRCA), Ancona. Italy.4Unit of Infectious Diseases, Annunziata Hospital, Cosenza. Italy.5Department of Clinical and Experimental Medicine, Unit of Geriatrics, University of Parma, Parma. Italy.6Department of Clinical and Experimental Medicine, University of Messina. Italy. Abstract OBJECTIVE: We aimed at summarizing current evidence about mechanisms for potentially harmful effects of proton pump inhibitors (PPIs). METHODS: A Pubmed search was performed, and 207 studies concerning the relationship between use of PPIs and cardiovascular diseases, kidney impairment, nutritional disorders, fractures, infections, functional decline, and mortality were selected and reviewed. RESULTS: PPIs may cause potentially harmful effects by several mechanisms, including endothelial dysfunction, hypomagnesemia, drug interactions, reduced absorption of selected nutrients, increased gastric microbiota and small intestine bacterial overgrowth, reduced immune response, tubular-interstitial inflammation, increased bone turnover, accumulation of amyloid in the brain. Clinical and epidemiologic evidence is not consistent in regard to some negative outcomes during PPI treatment. Data from randomized clinical trials seem to deny most of them, but they are usually designed to investigate efficacy of drugs in ideal conditions and are not powered enough to detect adverse events. Besides being at special risk of experiencing negative outcomes during long-term treatment with PPIs, older and complex patients treated with polypharmacy regimens are persistently excluded from randomized clinical trials. Thus, large observational studies involving real-world patients should be considered as an important informative source about potential risks related to PPIs. CONCLUSIONS: Current evidence suggests that use of PPIs may be associated with negative outcomes by eliciting several different pathophysiologic mechanisms. While short-term PPIs could be considered effective and safe in adult patients with acid-related disorders, their long-term and often inappropriate use in patients carrying vulnerability to adverse events and/or high risk of drug-interactions should be avoided. Copyright© Bentham Science Publishers; For any queries, please email at epub@benthamscience.org. KEYWORDS: Clostridium Difficile; Proton pump inhibitors; acute interstitial nephritis; cardiovascular risk; dementia.; fractures; hypomagnesemia; pneumonia; vitamin B12 Endothelial Function Scientific Update Sponsored by Endothelix Inc.


Comments