Amazing animal models of coronary microvascular (endothelial) dysfunction and how they can help our
- heartlung
- Jan 16, 2023
- 2 min read

Cardiovasc Res. 2020 Jan 11.
Experimental Animal Models of Coronary Microvascular Dysfunction.
Sorop O1, van de Wouw J1, Chandler S2, Ohanyan V2, Tune JD3, Chilian WM2, Merkus D1,4,5, Bender SB6,7,8, Duncker DJ1.
1 Division of Experimental Cardiology, Department of Cardiology, Erasmus MC, University Medical Center Rotterdam.
2 Department of Integrative Medical Sciences, Northeast Ohio Medical University, Rootstown, Ohio, USA.
3 Department of Anatomy, Cell Biology & Physiology, Indiana University School of Medicine, 635 Barnhill Drive, Indianapolis, Indiana, USA.
4 Walter Brendel Centre of Experimental Medicine, University Hospital, LMU Munich, Marchioninistr. 27, Munich, Germany.
5 German Center for Cardiovascular Research (DZHK), Partner Site Munich, Munich Heart Alliance (MHA), Munich, Germany.
6 Department of Biomedical Sciences, University of Missouri, Columbia, Missouri, USA.
7 Research Service, Harry S Truman Memorial Veterans Hospital, Columbia, Missouri, USA.
8 Dalton Cardiovascular Research Center, University of Missouri, Columbia, Missouri, USA.
Abstract
Coronary microvascular dysfunction (CMD) is commonly present in patients with metabolic derangements and is increasingly recognized as an important contributor to myocardial ischemia, both in the presence and absence of epicardial coronary atherosclerosis. The latter condition is termed ‘ischemia with non-obstructive coronary arteries’ (INOCA). Notwithstanding the high prevalence of INOCA, effective treatment remains elusive. Although to date there is no animal model for INOCA, animal models of CMD, one of the hallmarks of INOCA, offer excellent test models for enhancing our understanding of the pathophysiology of CMD and for investigating novel therapies. This article presents an overview of currently available experimental models of CMD – with an emphasis on metabolic derangements as risk factors – in dogs, swine, rabbits, rats and mice. In all the available animal models, metabolic derangements are most often induced by a high fat diet and/or diabetes mellitus via injection of alloxan or streptozotocin, but there is also a wide variety of spontaneous as well as transgenic animal models which develop metabolic derangements. Depending on number, severity and duration of exposure to risk factors – all these animal models show perturbations in coronary microvascular (endothelial) function and structure, similar to what has been observed in patients with INOCA and co-morbid conditions. The use of these animal models will be instrumental in identifying novel therapeutic targets and for the subsequent development and testing of novel therapeutic interventions to combat ischemic heart disease, the number one cause of death worldwide.
© The Author(s) 2020. Published by Oxford University Press on behalf of the European Society of Cardiology.



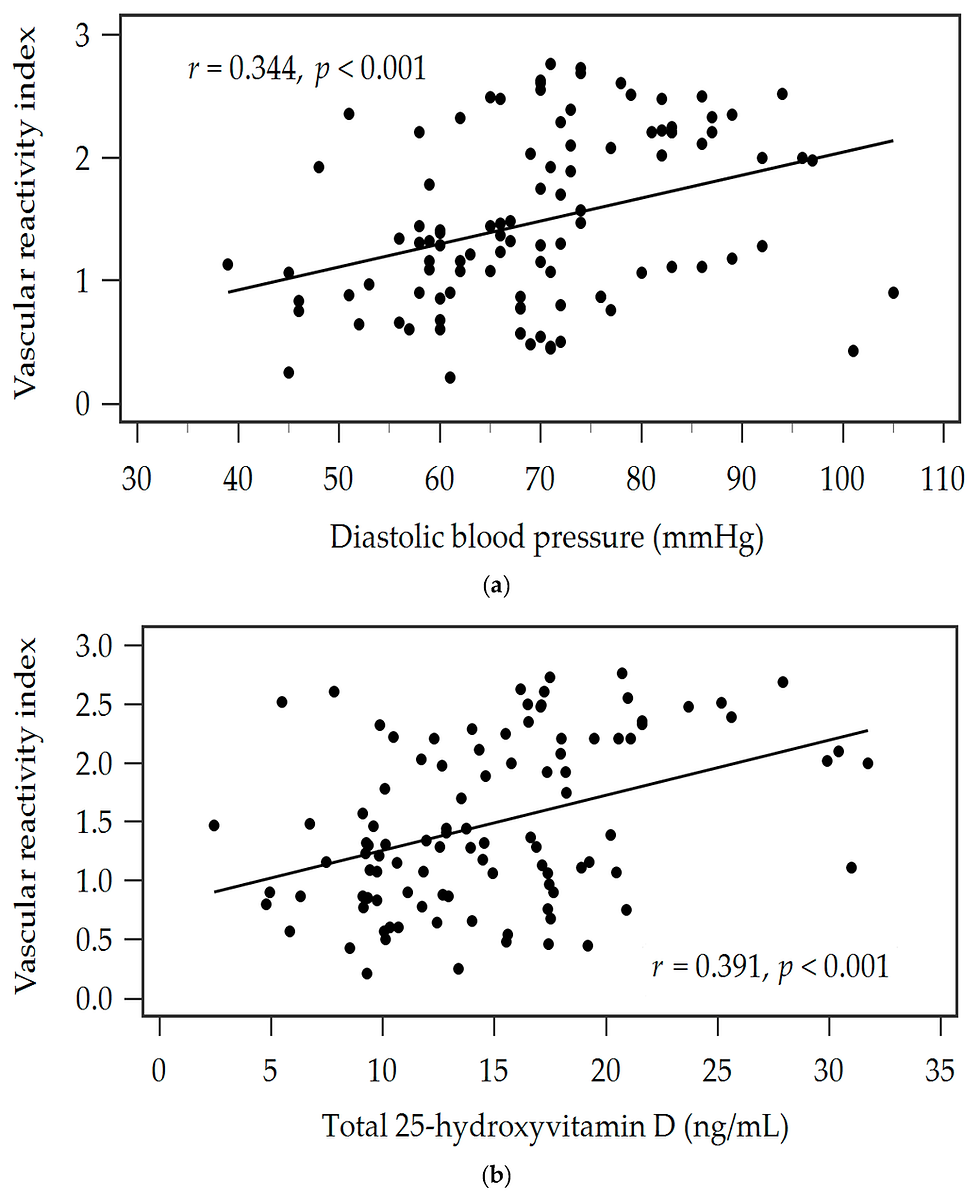
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)
Comments