Children with Type 1 Diabetes Have Delayed Flow-Mediated Dilation,
- heartlung
- Jan 16, 2023
- 3 min read
and Microvascular ED in Endocarditis
Can J Diabetes. 2017 Jul 25. pii: S1499-2671(16)30817-6. doi: 10.1016/j.jcjd.2017.06.011. [Epub ahead of print] Children with Type 1 Diabetes Have Delayed Flow-Mediated Dilation. Pillay S1, Anderson J2, Couper J2, Maftei O3, Gent R4, Peña AS2. Author information 1Robinson Research Institute and Discipline of Paediatrics, The University of Adelaide, Adelaide, South Australia, Australia; Endocrinology and Diabetes Centre, Women’s and Children’s Hospital, North Adelaide, South Australia, Australia. Electronic address: sarveshinee.pillay@gmail.com.2Robinson Research Institute and Discipline of Paediatrics, The University of Adelaide, Adelaide, South Australia, Australia; Endocrinology and Diabetes Centre, Women’s and Children’s Hospital, North Adelaide, South Australia, Australia.3Endocrinology and Diabetes Centre, Women’s and Children’s Hospital, North Adelaide, South Australia, Australia.4Medical Imaging, Women’s and Children’s Hospital, North Adelaide, South Australia, Australia. Abstract OBJECTIVES: Children with type 1 diabetes have accelerated atherosclerosis with early endothelial dysfunction as measured by reduced flow-mediated dilation (FMD) at 60 seconds postischemic stress (early FMD). Delayed dilation may also occur in the presence of cardiovascular risk factors and may be a more sensitive marker. No data exist that evaluate FMD beyond 60 seconds (delayed FMD) in children with type 1 diabetes. We aimed to compare early and delayed FMD in children with type 1 diabetes and in healthy children. METHODS: We studied 66 children 13.5±2.8 years of age; 29 were males. Of the 66 children, 38 had type 1 diabetes, and 28 were healthy age- and gender-matched controls. Evaluation of brachial artery FMD was performed at 60 seconds (FMD60s) and 120 seconds (FMD120s) postischemic stress. Early FMD was defined as peak FMD60s and delayed FMD as peak FMD120s. RESULTS: Children with type 1 diabetes had diabetes durations of 5.4±4.6 years and median glycated hemoglobin levels of 8.8 (6.6 to 14)% (73 [49 to 130] mmol/mol). Of the children, 8 with type 1 diabetes and 1 healthy child had delayed FMD; a relationship was seen between the prevalence of early FMD and delayed FMD in children with type 1 diabetes and healthy children, respectively (p=0.019). Children with type 1 diabetes and delayed FMD had lower FMD60s than children without delayed FMD (2.50±3.61 vs. 6.14±3.83 percentage units; p=0.02). Children with type 1 diabetes had lower FMD60s than healthy children (5.38±4.0 percentage units; p=0.03) but not FMD120s (7.56±3.5 percentage units; p=0.47). CONCLUSIONS: Delayed FMD patterns occur in children with type 1 diabetes and detect children who have more severe vascular abnormalities. The standard FMD60s remains the better marker to identify children at increased risk for cardiovascular disease. Copyright © 2017 Diabetes Canada. Published by Elsevier Inc. All rights reserved. KEYWORDS: children; diabète de type 1; dilatation induite par le flux; enfants; flow-mediated dilation; type 1 diabetes BMC Res Notes. 2017 Jul 28;10(1):342. doi: 10.1186/s13104-017-2660-3. Barcelos A1, Lamas C1,2,3, Tibiriça E4,5. Evaluation of microvascular function in patients with infective endocarditis using laser speckle contrast imaging and skin video-capillaroscopy: Author information 1National Institute of Cardiology, Ministry of Health, Rio de Janeiro, Brazil.2National Institute of Infectious Diseases Evandro Chagas, Oswaldo Cruz Institute, Rio de Janeiro, Brazil.3Unigranrio University, Rio de Janeiro, Brazil.4National Institute of Cardiology, Ministry of Health, Rio de Janeiro, Brazil. etibi@ioc.fiocruz.br.5Laboratory of Cardiovascular Investigation, Oswaldo Cruz Institute, Av. Brasil 4365, Rio de Janeiro, 21045-900, Brazil. etibi@ioc.fiocruz.br. Abstract OBJECTIVE: Infective endocarditis is a severe condition with high in-hospital and 5-year mortality. There is increasing incidence of infective endocarditis, which may be related to healthcare and changes in prophylaxis recommendations regarding oral procedures. Few studies have evaluated the microcirculation in patients with infective endocarditis, and so far, none have utilized laser-based technology or evaluated functional capillary density. The aim of the study is to evaluate the changes in the systemic microvascular bed of patients with both acute and subacute endocarditis. This is a cohort study that will include adult patients with confirmed active infective endocarditis according to the modified Duke criteria who were admitted to our center for treatment. A control group of sex- and age-matched healthy volunteers will be included. Functional capillary density, which is defined as the number of spontaneously perfused capillaries per square millimeter of skin, will be assessed by video-microscopy with an epi-illuminated fiber optic microscope. Capillary recruitment will be evaluated using post-occlusive reactive hyperemia. Microvascular flow will be evaluated in the forearm using a laser speckle contrast imaging system for the noninvasive and continuous measurement of cutaneous microvascular perfusion changes. Laser speckle contrast imaging will be used in combination with skin iontophoresis of acetylcholine, an endothelium-dependent vasodilator, or sodium nitroprusside (endothelium independent) to test microvascular reactivity. RESULTS: The present study will contribute to the investigation of microcirculatory changes in infective endocarditis and possibly lead to an earlier diagnosis of the condition and/or determination of its severity and complications. Trial registration ClinicalTrials.gov ID: NCT02940340. KEYWORDS: Infective endocarditis; Microcirculation; Microvascular dysfunction; Skin video-capillaroscopy; Speckle contrast imaging Endothelial Function Scientific Update Sponsored by Endothelix Inc.
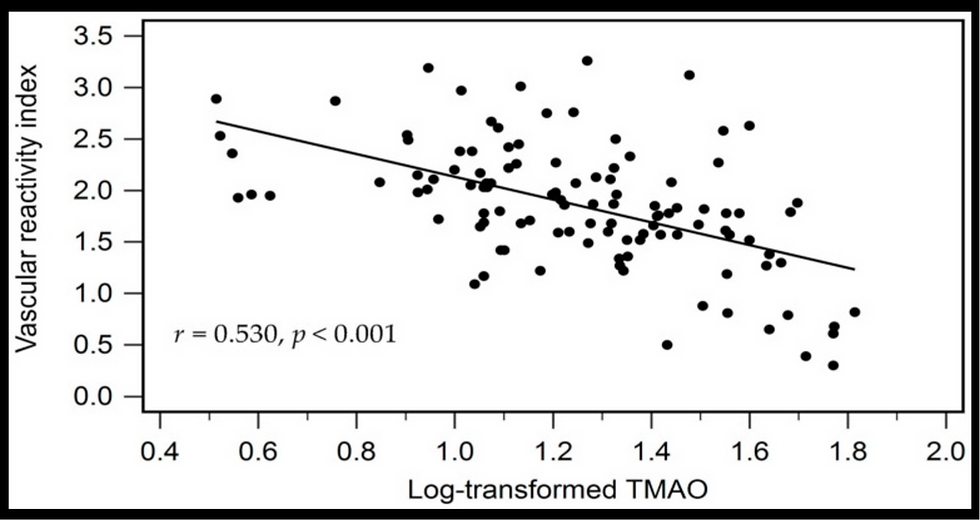
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments