Endothelial dysfunction in children with obstructive sleep apnea syndrome
- heartlung
- Jan 16, 2023
- 2 min read

Endothelial dysfunction in children with obstructive sleep apnea syndrome
Xu ZF1, Zhang FJ2, Ge WT3, Feng GS4, Wu YX5, Ni X3.
Author information
1 Department of Respiratory Medicine, Beijing Children’s Hospital, Capital Medical University, Beijing 100045, China.
2 Department of Comprehensive Ward, Beijing Children’s Hospital, Capital Medical University, Beijing 100045, China.
3 Department of Otolaryngology, Head & Neck Surgery, Beijing Children’s Hospital, Capital Medical University, Beijing 100045, China.
4 Research Center for Big Data and Engineering, Beijing Children’s Hospital, Capital Medical University, Beijing 100045, China.
5 Beijing Key Laboratory of Pediatric Otolaryngology, Head & Neck Surgery, Beijing Children’s Hospital, Capital Medical University, Beijing 100045, China. nixin@bch.com.cn
Abstract
Objective: To evaluate the endothelial function in obstructive sleep apnea syndrome(OSAS) children and to identify related factors of endothelial dysfunction.
Methods: This was a cross-sectional study. Children with habitual snoring (snoring ≥3 nights per week) admitted to the ward of otolaryngology, head and neck surgery, Beijing Children’s Hospital were recruited to this study between 1(st) June 2015 and 1(st) March 2016. All children aged 3 to 11 years and of them 245 were boys and 110 were girls. All subjects underwent an overnight polysomnography (PSG), as well as endothelial function testing. All subjects were grouped into primary snoring (PS) and OSAS group according to the obstructive apnea hypopnea index (OAHI). T test or Wilcoxon test were used to compare the differences in PSG results between the two groups, and univariate and multivariate correlation analyses were used to explore the relevant factors affecting the endothelial function.
Results: A total of 355 subjects were enrolled and 248 had OSAS, and 107 had PS. There were no significant differences in age, gender and body mass index (BMI) Z-score between the two groups (all P>0.05). OSAS group had higher OAHI, oxgen desaturation index and respiratory related arousal index (5.2 (2.2, 13.2) vs. 0.4 (0.1, 0.7), 4.1 (2.0, 13.1) vs. 0.5 (0.1, 1.0), 2.5 (1.0, 4.8) vs. 0.4 (0.1, 0.9), Z=-14.957, -11.790, -10.378, all P<0.01), and lower minimum oxygen saturation and reactive hyperemia index (RHI) than those of PS (0.89 (0.85, 0.92) vs. 0.94 (0.91, 0.95), 1.2±0.2 vs. 1.1±0.1, Z=-9.337, t=5.354, P<0.01). Univariate regression analysis showed that RHI was linearly correlated with age (parameter estimate=0.017, P<0.01), gender (parameter estimate=0.065, P<0.01), OAHI (parameter estimate=-0.023, P<0.01), oxygen desaturation index (parameter estimate=-0.019, P<0.01), respiratory related arousal index (parameter estimate=-0.031, P<0.01), and oxygen saturation nadir (parameter estimate=0.067, P=0.045). The relationship between BMI Z-score and RHI was quadratic. Multivariate regression analysis showed that age (parameter estimate=0.015, P<0.01), BMI Z-score (parameter estimate=0.040, P<0.01), BMI Z-score quadratic form (parameter estimate=-0.010, P<0.01), respiratory related arousal index (parameter estimate=-0.020, P<0.01) were independently correlated with RHI.
Conclusions: Children with OSAS have significant endothelial dysfunction compared with PS. Frequent arousals due to obstructive respiratory events during sleep may be a candidate risk factor for endothelial dysfunction in children with OSAS.
KEYWORDS:
Arousal; Child; Endothelial cells; Sleep apnea, obstructive
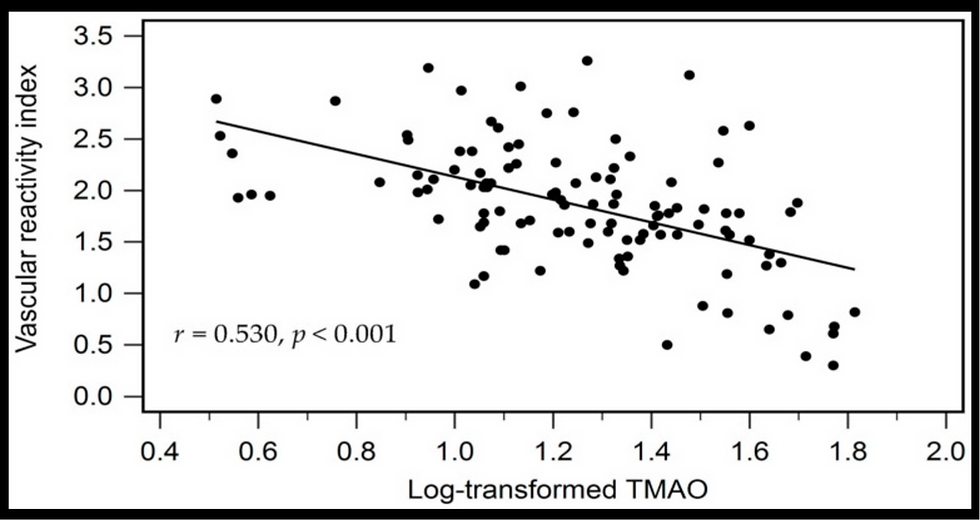
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments