Endothelial Dysfunction Linked to Alzheimer, Pulmonary Vasculitis, Retinopathy, and Acute Stroke
- Jan 16, 2023
- 5 min read
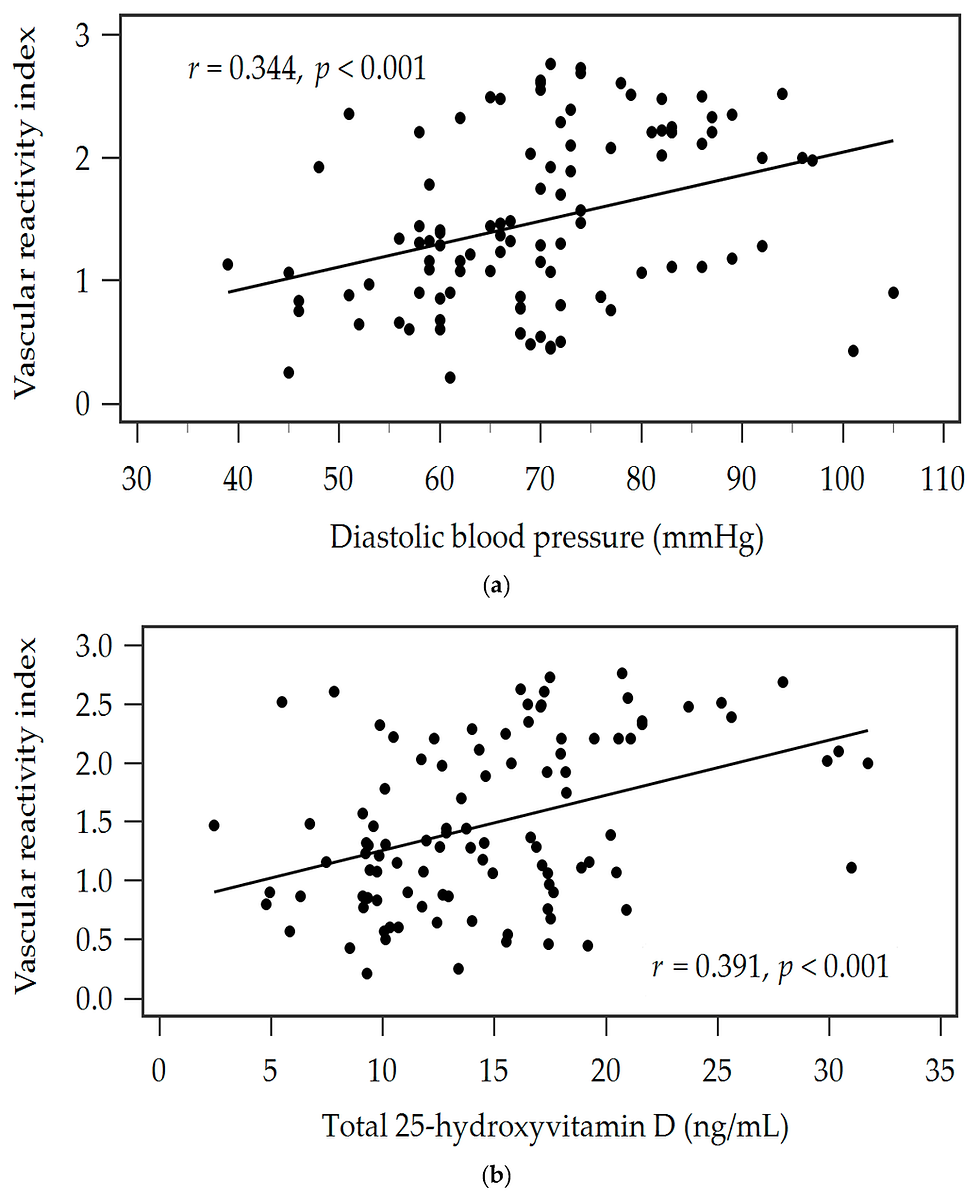
Int J Mol Sci. 2017 Sep 13;18(9). pii: E1965. doi: 10.3390/ijms18091965. Blood-Brain Barrier Dysfunction and the Pathogenesis of Alzheimer’s Disease. Yamazaki Y1, Kanekiyo T2. Author information 1Department of Neuroscience, Mayo Clinic, 4500 San Pablo Road, Jacksonville, FL 32224, USA. yamazaki.yu@mayo.edu.2Department of Neuroscience, Mayo Clinic, 4500 San Pablo Road, Jacksonville, FL 32224, USA. kanekiyo.takahisa@mayo.edu. Abstract Brain capillary endothelial cells form the blood-brain barrier (BBB), which is covered with basement membranes and is also surrounded by pericytes and astrocyte end-feet in the neurovascular unit. The BBB tightly regulates the molecular exchange between the blood flow and brain parenchyma, thereby regulating the homeostasis of the central nervous system (CNS). Thus, dysfunction of the BBB is likely involved in the pathogenesis of several neurological diseases, including Alzheimer’s disease (AD). While amyloid-β (Aβ) deposition and neurofibrillary tangle formation in the brain are central pathological hallmarks in AD, cerebrovascular lesions and BBB alteration have also been shown to frequently coexist. Although further clinical studies should clarify whether BBB disruption is a specific feature of AD pathogenesis, increasing evidence indicates that each component of the neurovascular unit is significantly affected in the presence of AD-related pathologies in animal models and human patients. Conversely, since some portions of Aβ are eliminated along the neurovascular unit and across the BBB, disturbing the pathways may result in exacerbated Aβ accumulation in the brain. Thus, current evidence suggests that BBB dysfunction may causatively and consequently contribute to AD pathogenesis, forming a vicious cycle between brain Aβ accumulation and neurovascular unit impairments during disease progression. KEYWORDS: amyloid-β; astrocytes; basement membrane; cerebral amyloid angiopathy; endothelial cells; neurovascular unit; pericytes; tight junctions Full-text Arterioscler Thromb Vasc Biol. 2017 Sep;37(9):e108-e114. doi: 10.1161/ATVBAHA.117.309813. Peripheral Arterial Tonometry in Pulmonary Vasculitis. Falkowski A1, Wardyn KA2, Życińska K2. Author information 1Department of Family Medicine, Internal and Metabolic Diseases, Warsaw Medical University, and Systemic Vasculitis Outpatient Clinic Czerniakowski Hospital, Warsaw, Poland. a.falkowski.ptmr@gmail.com.2Department of Family Medicine, Internal and Metabolic Diseases, Warsaw Medical University, and Systemic Vasculitis Outpatient Clinic Czerniakowski Hospital, Warsaw, Poland. Abstract Vascular wall inflammation in primary vasculitides results in diminished vessel dilation and finally impaired blood flow, causing multiple organs dysfunction and ultimate damage. In granulomatosis with polyangiitis (GPA), the inflammatory process concerns small and medium sized vessels and its pulmonary location is often predominant. The pivotal role in the development of that pathology plays vascular endothelium. Endothelial vasodilatory function strongly depends on the instant production and release of nitrogen oxide (NO), a potent local factor controlling vascular tonus. NO output is triggered by a variety of stimuli, especially by ischemia. The endothelial vasodilatory ability can be measured indirectly by a few of methods, one of them is peripheral arterial tonometry (PAT). The method assesses reactive hyperemia, mediated mostly by NO release, as a response to vessel occlusion. The vasodilatory reaction depends on the quality of the endotheliumwhich deteriorates with time of GPA disease progression. The aim of the present study was to estimate a correlation between the clinical status, reflected by the disease extent index (DEI), and the vasodilatory endothelial function reflected by the index of arterial reactive hyperemia (RHI), measured by PAT in 27 patients with GPA, having a significant pulmonary involvement. We found a moderate inverse correlation between DEI and log-transformed RHI (r = -0.46 p < 0.05). The conclusion is that impaired endothelial function, as assessed by RHI-PAT, might predict the GPA progression. KEYWORDS: Endotheium; Granulomatosis; Inflammation; Polyangiitis; Pulmonary vasculitis; Tonometry; Vascular wall; Vasodilation Invest Ophthalmol Vis Sci. 2017 Sep 1;58(11):4524-4529. doi: 10.1167/iovs.17-21825. Peripheral Vascular Endothelial Dysfunction in Central Serous Chorioretinopathy. Wang NK1,2, Fu Y2,3, Wang JP4,5, Kang EY1,2, Wu AL1,2, Tseng YJ6, Yeh LK1,2, Chen KJ1,2, Wu WC1,2, Ho WJ2,7, Lai CC1,2. Author information 1Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou Medical Center, Taoyuan, Taiwan.2College of Medicine, Chang Gung University, Taoyuan, Taiwan.3Department of Dermatology, Chang Gung Memorial Hospital, Linkou Medical Center, Taoyuan, Taiwan.4Department of Orthopaedics and Traumatology, Taipei Veterans General Hospital, Taipei, Taiwan.5School of Medicine, National Yang-Ming University, Taipei, Taiwan.6Herbert Irving Comprehensive Cancer Center, Columbia University, New York, New York, United States.7Department of Cardiology, Chang Gung Memorial Hospital, Linkou Medical Center, Taoyuan, Taiwan. Abstract PURPOSE: To explore the pathophysiology of central serous chorioretinopathy (CSC) by comparing peripheral vascular endothelium function in patients with CSC and control subjects. METHODS: This study included 34 patients with CSC who attended the Department of Ophthalmology and 34 healthy age- and sex-matched healthy control subjects from a routine physical check-up population. Endothelium-dependent flow-mediated vasodilation (FMD) and endothelium-independent nitroglycerine-mediated vasodilation (NMD) were measured using high-resolution, two-dimensional ultrasonographic imaging of the brachial artery. Blood samples were taken to test serum glucose, cholesterol, triglyceride, alanine aminotransferase, uric acid, and high-sensitivity C-reactive protein (hs-CRP) levels. RESULTS: The mean age of patients with CSC was 44.0 years (SD ±8.1) and that of controls 46.1 years (±9.9) (P = 0.352). There were no significant differences between groups in serum biochemical data, including serum glucose, alanine aminotransferase, uric acid, cholesterol, triglyceride, and hs-CRP. FMD was significantly impaired in patients with CSC compared with control subjects (CSC: 4.62 ± 1.96, control: 7.52 ± 2.63, P < 0.001), whereas NMD did not differ significantly between the two groups (CSC: 16.31 ± 5.60, control: 16.22 ± 5.56, P = 0.950). CONCLUSIONS: This study demonstrated impaired FMD in patients with CSC and the results have provided evidence of peripheral endothelium dysfunction associated with CSC in patients. J Am Heart Assoc. 2017 Sep 11;6(9). pii: e006010. doi: 10.1161/JAHA.117.006010. Sleep-Disordered Breathing in Acute Ischemic Stroke: A Mechanistic Link to Peripheral Endothelial Dysfunction. Scherbakov N1, Sandek A2, Ebner N2, Valentova M2, Nave AH3, Jankowska EA4,5, Schefold JC6, von Haehling S2, Anker SD2, Fietze I7, Fiebach JB3, Haeusler KG3,8, Doehner W3,9. Author information 1Center for Stroke Research Berlin (CSB), Charité-Universitätsmedizin Berlin, Berlin, Germany nadja.scherbakov@charite.de.2Innovative Clinical Trials, Department of Cardiology and Pneumology, University Medicine Goettingen (UMG), Goettingen, Germany.3Center for Stroke Research Berlin (CSB), Charité-Universitätsmedizin Berlin, Berlin, Germany.4Department of Heart Diseases, Wroclaw Medical University, Wroclaw, Poland.5Cardiology Department, Military Hospital, Wroclaw, Poland.6Department of Intensive Care Medicine, Inselspital, University Hospital of Bern, Switzerland.7Interdisciplinary Center of Sleep Medicine, Charité-Universitätsmedizin Berlin, Berlin, Germany.8Department of Neurology, Charité-Universitätsmedizin Berlin, Berlin, Germany.9Department of Cardiology, Charité-Universitätsmedizin Berlin, Berlin, Germany. Abstract BACKGROUND: Sleep-disordered breathing (SDB) after acute ischemic stroke is frequent and may be linked to stroke-induced autonomic imbalance. In the present study, the interaction between SDB and peripheral endothelial dysfunction (ED) was investigated in patients with acute ischemic stroke and at 1-year follow-up. METHODS AND RESULTS: SDB was assessed by transthoracic impedance records in 101 patients with acute ischemic stroke (mean age, 69 years; 61% men; median National Institutes of Health Stroke Scale, 4) while being on the stroke unit. SDB was defined by apnea-hypopnea index ≥5 episodes per hour. Peripheral endothelial function was assessed using peripheral arterial tonometry (EndoPAT-2000). ED was defined by reactive hyperemia index ≤1.8. Forty-one stroke patients underwent 1-year follow-up (390±24 days) after stroke. SDB was observed in 57% patients with acute ischemic stroke. Compared with patients without SDB, ED was more prevalent in patients with SDB (32% versus 64%; P<0.01). After adjustment for multiple confounders, presence of SDB remained independently associated with ED (odds ratio, 3.1; [95% confidence interval, 1.2-7.9]; P<0.05). After 1 year, the prevalence of SDB decreased from 59% to 15% (P<0.001). Interestingly, peripheral endothelial function improved in stroke patients with normalized SDB, compared with patients with persisting SDB (P<0.05). CONCLUSIONS: SDB was present in more than half of all patients with acute ischemic stroke and was independently associated with peripheral ED. Normalized ED in patients with normalized breathing pattern 1 year after stroke suggests a mechanistic link between SDB and ED. Endothelial Function Scientific Update Sponsored by Endothelix Inc.


Comments