Fingertip Reactive Hyperemia Peripheral Arterial Tonometry Score Predicts Response to Biventricular
- heartlung
- Jan 16, 2023
- 2 min read
Fingertip Reactive Hyperemia Peripheral Arterial Tonometry Score Predicts Response to Biventricular Pacing.
Okutucu S1, Jam F2, Sabanoglu C3, Yetis Sayin B1, Aksoy H1, Ercan Akgul E1, Oto A1
Abstract PURPOSE: The objectives of this study were to: (i) evaluate endothelial function via fingertip reactive hyperemia peripheral arterial tonometry (RH-PAT) among heart failure (HF) patients receiving cardiac resynchronization therapy (CRT), (ii) assess the effects of CRT on RH-PAT score, and (iii) investigate whether RH-PAT score can identify CRT response. METHODS: A total of 63 patients (61.8 ± 10.3 years; 50 males; left ventricular (LV) ejection fraction 24.3 ± 3.9%) with HF who received CRT were enrolled. Endothelial function via RH-PAT was assessed 1 day before and 6 months after CRT. Minnesota Living with Heart Failure Questionnaire (MLWHFQ) was used to assess clinical improvements. CRT response was defined as a reduction in LV end-systolic volume ≥ 15% at 6 months. RESULTS: A RH-PAT score of < 1.7 signified a cut-off for endothelial dysfunction (ED). Baseline ED was observed among 43 (68.3%) patients and was more prevalent in responders (76.1% vs. 47.1%, p = 0.037). RH-PAT score improved 6 months after CRT (1.58 ± 0.35 vs. 1.71 ± 0.31, p = 0.012). A RH-PAT score of < 1.7 was a significant independent predictor of CRT response in multivariate logistic regression analysis (beta = 1.275, OR = 3.512, 95% CI = 1.231-11.477, p = 0.032). The severity of ED was an independent predictor of LV reverse remodeling (beta = -8.873, p = 0.015). Spearman’s correlation analysis revealed moderate positive correlations between an improvement in RH-PAT (delta RH-PAT) and LV reverse remodeling (r = 0.461, p = 0.001) and MLWHFQ score (r = 0.440, p = 0.001). CONCLUSIONS: ED detected via RH-PAT could predict the response to CRT. The RH-PAT score increased 6 months after CRT and was correlated with echocardiographic and clinical improvements. Full-Text
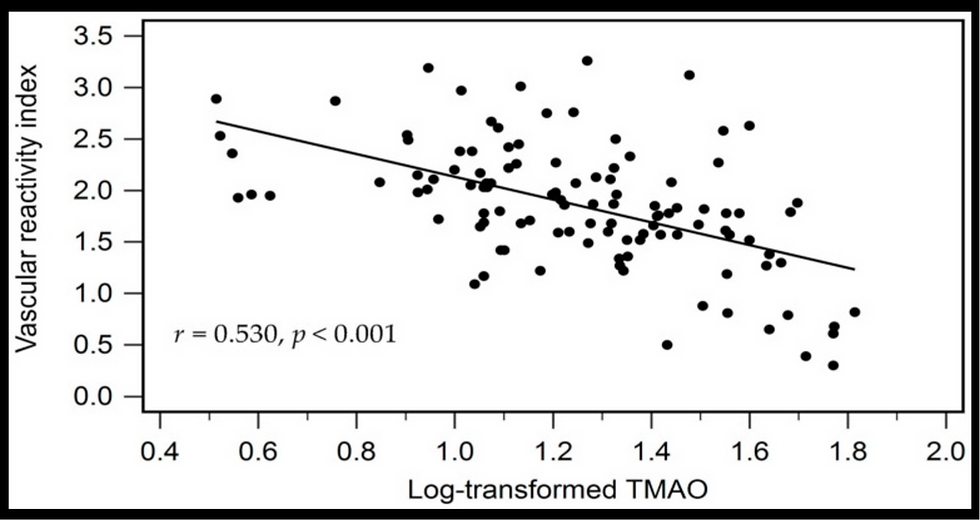
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments