Hypertension, Thrombosis, Kidney Failure, and Diabetes:
- heartlung
- Jan 16, 2023
- 2 min read
Is COVID-19 an Endothelial Disease? A Comprehensive Evaluation of Clinical and Basic Evidence.
J Clin Med. 2020 May 11;9(5) Hypertension, Thrombosis, Kidney Failure, and Diabetes: Is COVID-19 an Endothelial Disease? A Comprehensive Evaluation of Clinical and Basic Evidence. Sardu C1,2, Gambardella J3,4, Morelli MB4,5, Wang X4, Marfella R1, Santulli G3,4,5. Author information 1 Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, 80100 Naples, Italy. 2 Department of Medical Sciences, International University of Health and Medical Sciences “Saint Camillus”, 00131 Rome, Italy. 3 Department of Advanced Biomedical Sciences, International Translational Research and Medical Education Academic Research Unit (ITME), “Federico II” University, 80131 Naples, Italy. 4 Department of Medicine, Division of Cardiology, Albert Einstein College of Medicine, Wilf Family Cardiovascular Research Institute, New York, NY 10461, USA. 5 Department of Molecular Pharmacology, Fleischer Institute for Diabetes and Metabolism (FIDAM), Montefiore University Hospital, New York, NY 10461, USA. Abstract The symptoms most commonly reported by patients affected by coronavirus disease (COVID-19) include cough, fever, and shortness of breath. However, other major events usually observed in COVID-19 patients (e.g., high blood pressure, arterial and venous thromboembolism, kidney disease, neurologic disorders, and diabetes mellitus) indicate that the virus is targeting the endothelium, one of the largest organs in the human body. Herein, we report a systematic and comprehensive evaluation of both clinical and preclinical evidence supporting the hypothesis that the endothelium is a key target organ in COVID-19, providing a mechanistic rationale behind its systemic manifestations. KEYWORDS: ACE2, acute kidney injury; COVID; Kawasaki disease; blood pressure; catepsin; coronavirus; cytokine storm; endothelium; heparin

Figure 1. Endothelial dysfunction is a major determinant of COVID-19. The SARS-CoV-2 coronavirus accesses host cells via the binding of its spike glycoprotein to angiotensin-converting enzyme 2 (ACE2), sialic acid receptor, transmembrane serine protease 2 (TMPRSS2), and extracellular matrix metalloproteinase inducer (CD147); catepsin B and L also participate in virus entry. All of these factors are expressed in endothelial cells. Endothelial dysfunction is a common feature of the clinical manifestations observed in COVID-19 patients. All of the drugs proposed as a potential therapeutic strategy to treat COVID-19 patients have been shown to improve endothelial function, including tocilizumab, colchicine, chloroquine/hydroxychloroquine, azithromycin, and famotidine (see text for details and references).

Figure 3. Clinical course of COVID-19 patients. Two main overlapping phases constitute the key pathogenic events in COVID-19: the acute phase represented by viral infection, followed by the immune/inflammatory response. Common clinical and laboratory findings are reported within the arrows at the bottom of the figure.
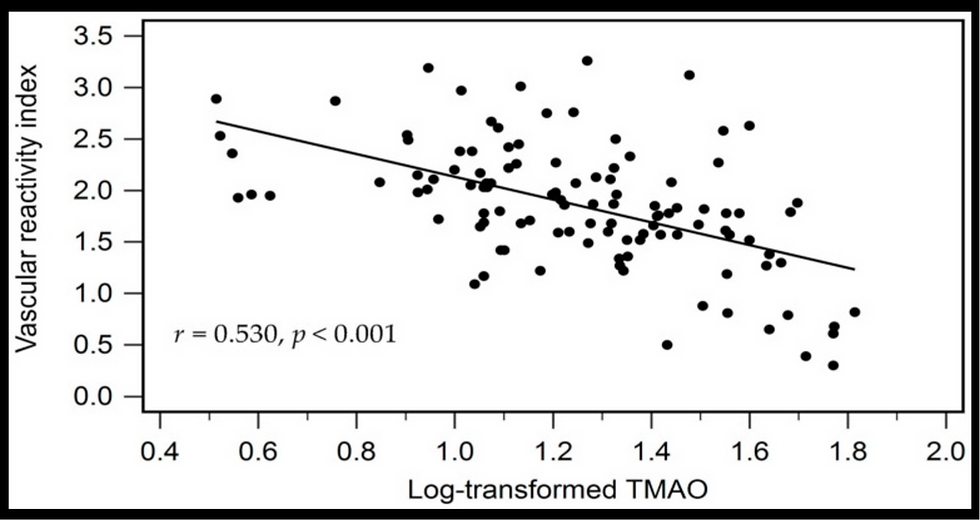
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments