Low fingertip temperature rebound measured by digital thermal monitoring strongly correlates with...
- Jan 9, 2023
- 3 min read
Low fingertip temperature rebound measured by digital thermal monitoring strongly correlates with the presence and extent of coronary artery disease diagnosed by 64-slice multi-detector computed tomography
Naser Ahmadi, Vahid Nabavi, Vivek Nuguri, Fereshteh Hajsadeghi, Ferdinand Flores, Mohammad Akhtar, Stanley Kleis, Harvey Hecht, Morteza Naghavi, Matthew Budoff
Int J Cardiovasc Imaging 2009 Oct;25(7):725-38.
Abstract
Previous studies showed strong correlations between low fingertip temperature rebound measured by digital thermal monitoring (DTM) during a 5 min arm-cuff induced reactive hyperemia and both the Framingham Risk Score (FRS), and coronary artery calcification (CAC) in asymptomatic populations. This study evaluates the correlation between DTM and coronary artery disease (CAD) measured by CT angiography (CTA) in symptomatic patients. It also investigates the correlation between CTA and a new index of neurovascular reactivity measured by DTM. 129 patients, age 63 +/- 9 years, 68% male, underwent DTM, CAC and CTA. Adjusted DTM indices in the occluded arm were calculated: temperature rebound: aTR and area under the temperature curve aTMP-AUC. DTM neurovascular reactivity (NVR) index was measured based on increased fingertip temperature in the non-occluded arm. Obstructive CAD was defined as >or=50% luminal stenosis, and normal as no stenosis and CAC = 0. Baseline fingertip temperature was not different across the groups. However, all DTM indices of vascular and neurovascular reactivity significantly decreased from normal to non-obstructive to obstructive CAD [(aTR 1.77 +/- 1.18 to 1.24 +/- 1.14 to 0.94 +/- 0.92) (P = 0.009), (aTMP-AUC: 355.6 +/- 242.4 to 277.4 +/- 182.4 to 184.4 +/- 171.2) (P = 0.001), (NVR: 161.5 +/- 147.4 to 77.6 +/- 88.2 to 48.8 +/- 63.8) (P = 0.015)]. After adjusting for risk factors, the odds ratio for obstructive CAD compared to normal in the lowest versus two upper tertiles of FRS, aTR, aTMP-AUC, and NVR were 2.41 (1.02-5.93), P = 0.05, 8.67 (2.6-9.4), P = 0.001, 11.62 (5.1-28.7), P = 0.001, and 3.58 (1.09-11.69), P = 0.01, respectively. DTM indices and FRS combined resulted in a ROC curve area of 0.88 for the prediction of obstructive CAD. In patients suspected of CAD, low fingertip temperature rebound measured by DTM significantly predicted CTA-diagnosed obstructive disease.
Read Full Text Here: https://link.springer.com/article/10.1007/s10554-009-9476-8

Accompanying Editorial: Digital thermal monitoring of vascular function: a novel tool to improve cardiovascular risk assessment.
Khawar M Gul, Naser Ahmadi, Zhiying Wang, Craig Jamieson, Khurram Nasir, Ralph Metcalfe, Harvey S Hecht, Craig J Hartley, Morteza Naghavi
Vasc Med 2009 May;14(2):143-8.
Abstract
Digital thermal monitoring (DTM) of vascular function during cuff-occlusive reactive hyperemia relies on the premise that changes in fingertip temperature during and after an ischemic stimulus reflect changes in blood flow. To determine its utility in individuals with and without known coronary heart disease (CHD), 133 consecutive individuals (age 54 +/- 10 years, 50% male, 19 with known CHD) underwent DTM during and after 2 minutes of supra-systolic arm cuff inflation. Fingertip temperatures of the occluded and non-occluded fingertips were measured simultaneously. Post-cuff deflation temperature rebound (TR) was lower in the CHD patients and in those with an increased Framingham risk score (FRS) compared to the normal group. After adjustment for age, sex, and cardiac risk factors, TR was significantly lower in those with CHD compared to those without CHD (p < 0.05). This study demonstrates that vascular dysfunction measured by DTM is associated with CHD and an increased FRS, and could potentially be used to identify high-risk patients.
Read Full Text Here: https://journals.sagepub.com/doi/10.1177/1358863X08098850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed


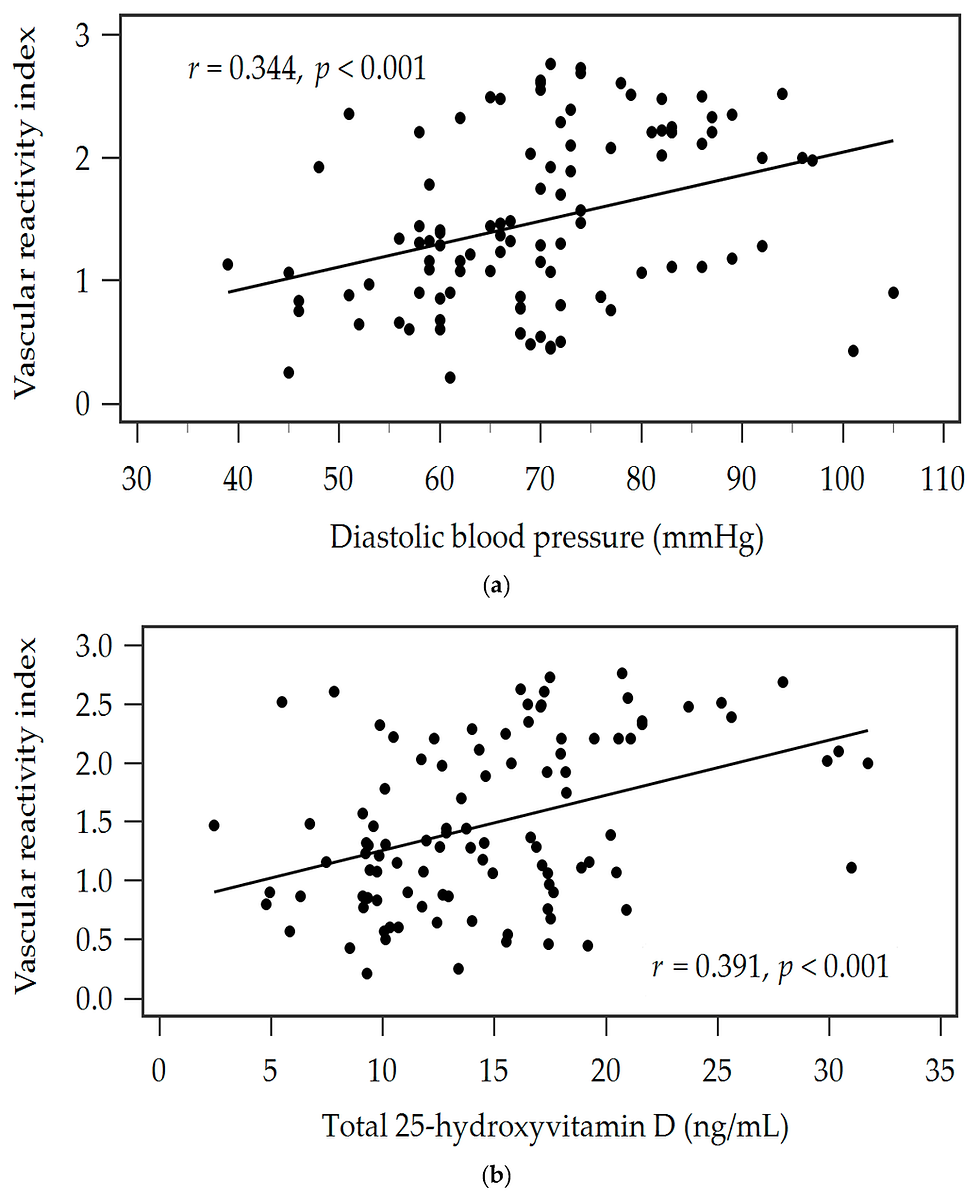
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)
Comments