Mayo Clinic Study Shows Assessment of Endothelial Function Predicts Future Risk of Cancer,
- heartlung
- Jan 16, 2023
- 2 min read
Indicating CVD and Cancer Share Endothelial Dysfunction

Eur J Prev Cardiol. 2019 Oct 31:2047487319884246. Assessment of peripheral endothelial function predicts future risk of solid-tumor cancer. Toya T1,2, Sara JD1, Corban MT1, Taher R1, Godo S1, Herrmann J1, Lerman LO3, Lerman A1. Author information 1 Department of Cardiovascular Medicine, Mayo Clinic, USA. 2 Division of Cardiology, National Defense Medical College, Japan. 3 Division of Nephrology and Hypertension, Mayo Clinic, USA. Abstract AIMS: Cardiovascular health metrics predict the risk not only of cardiovascular diseases but also of several types of cancers. Microvascular endothelial dysfunction can predict future cardiovascular adverse events, but the predictive value of microvascular endothelial dysfunction for future risk of solid-tumor cancer has not been characterized. METHODS: A total of 488 patients who underwent microvascular endothelial function assessment using reactive hyperemia peripheral arterial tonometry were included in this study. Microvascular endothelial dysfunction was defined as a reactive hyperemia peripheral arterial tonometry index ≤2.0. RESULTS: Of 221 patients with a baseline reactive hyperemia peripheral arterial tonometry index ≤2.0, 21 patients (9.5%) were diagnosed with incident solid-tumor cancer during follow-up, whereas of 267 patients with a baseline reactive hyperemia peripheral arterial tonometry index >2.0, 10 patients (3.7%) were diagnosed with incident solid-tumor cancer during follow-up (p = 0.009). Patients with a reactive hyperemia peripheral arterial tonometry index ≤2.0 had lower solid-tumor cancer-free survival compared to patients with a reactive hyperemia peripheral arterial tonometry index >2.0 (log-rank p = 0.017) (median follow-up 6.0 (3.0-9.1) years). Cox proportional hazard analyses showed that a reactive hyperemia peripheral arterial tonometry index ≤2.0 predicted the incidence of solid-tumor cancer, with a hazard ratio of 2.52 (95% confidence interval 1.17-5.45; p = 0.019) after adjusting for age, sex, and coronary artery disease, 2.83 (95% confidence interval 1.30-6.17; p = 0.009) after adjusting for diabetes mellitus, hypertension, smoking status, and body mass index >30 kg/m2, 2.79 (95% confidence interval 1.21-6.41; p = 0.016) after adjusting for fasting plasma glucose, systolic blood pressure, smoking status (current or former), and body mass index, and 2.43 (95% confidence interval 1.10-5.34; p = 0.028) after adjusting for Framingham risk score. CONCLUSION: Microvascular endothelial dysfunction, as defined by a reactive hyperemia peripheral arterial tonometry index ≤2.0, was associated with a greater than two-fold increased risk of solid-tumor cancer. Microvascular endothelial dysfunction may be a useful marker to predict the future risk of solid-tumor cancer, in addition to its known ability to predict cardiovascular disease. Further research is necessary to develop adequate cancer screening strategies for patients with microvascular endothelial dysfunction. KEYWORDS: Cardiovascular diseases; cancer; microvessel abnormalities; vascular endothelium-dependent relaxation View Full-Text


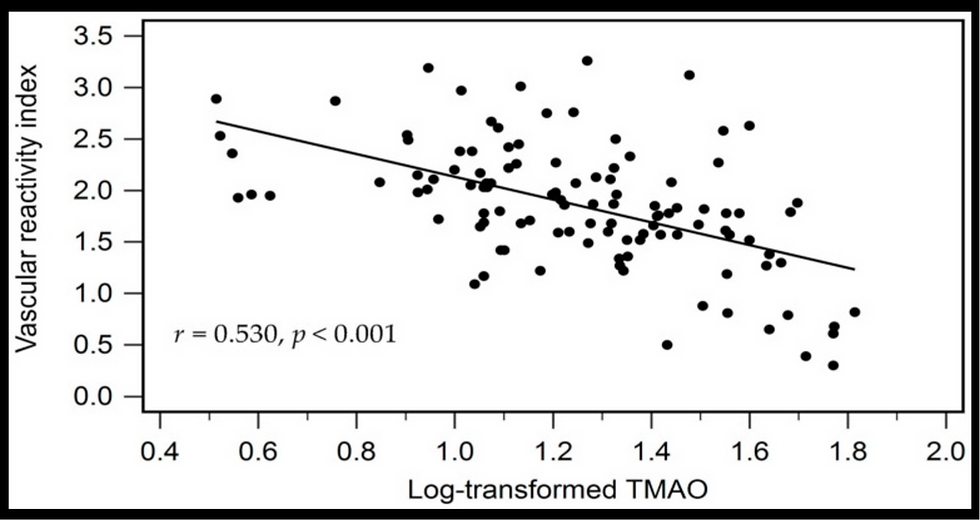
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments