Oxford Study Shows Endothelial Dysfunction Predicts Progression of Abdominal Aortic Aneurism (AAA)
- heartlung
- Jan 16, 2023
- 2 min read
Eur J Vasc Endovasc Surg. 2017 Apr 13. pii: S1078-5884(17)30157-0. doi: 10.1016/j.ejvs.2017.03.001. [Epub ahead of print]
Flow Mediated Dilatation and Progression of Abdominal Aortic Aneurysms.
Lee R1, Bellamkonda K2, Jones A2, Killough N2, Woodgate F2, Williams M2, Cassimjee I2, Handa A2; Oxford Abdominal Aortic Aneurysm Study2.
Collaborators (14)
Antonopoulos A, Antoniades C, Channon KM, Perera R, Hurst K, Milosevic I, Darby CR, Halliday A, Hands LJ, Lintott P, Magee TR, Northeast A, Perkins J, Sideso E.
1Nuffield Department of Surgical Sciences, University of Oxford, Oxford, UK. Electronic address: regent.lee@nds.ox.ac.uk.2Nuffield Department of Surgical Sciences, University of Oxford, Oxford, UK.
Abstract
OBJECTIVE/BACKGROUND:
Biomarker(s) for prediction of the future progression rate of abdominal aortic aneurysms (AAA) may be useful to stratify the management of individual patients. AAAs are associated with features of systemic inflammation and endothelial dysfunction. Flow mediated dilatation (FMD) of the brachial artery is a recognised non-invasive measurement for endothelial function. We hypothesised that FMD is a potential biomarker of AAA progression and reflects the temporal changes of endothelial function during AAA progression.
METHODS:
In a prospectively recruited cohort of patients with AAAs (Oxford Abdominal Aortic Aneurysm Study), AAA size was recorded by antero-posterior diameter (APD) (outer to outer) on ultrasound. Annual AAA progression was calculated by (ΔAPD/APD at baseline)/(number of days lapsed/365 days). FMD was assessed at the same time as AAA size measurement. Analyses of data were performed in the overall cohort, and further in subgroups of AAA by size (small: 30-39 mm; moderate: 40-55 mm; large: > 55 mm).
RESULTS:
FMD is inversely correlated with the diameter of AAAs in all patients (n=162, Spearman’s r=-.28, p 001). FMD is inversely correlated with AAA diameter progression in the future 12 months (Spearman’s r=-.35, p=.001), particularly in the moderate size group. Furthermore, FMD deteriorates during the course of AAA surveillance (from a median of 2.0% at baseline to 1.2% at follow-up; p=.004), while surgical repair of AAAs (n=50 [open repair n=22, endovascular repair n=28)] leads to an improvement in FMD (from 1.1% pre-operatively to 3.8% post-operatively; p 001), irrespective of the type of surgery.
CONCLUSION:
FMD is inversely correlated with future AAA progression in humans. FMD deteriorates during the natural history of AAA, and is improved by surgery. The utility of FMD as a potential biomarker in the context of AAA warrants further investigation
Endothelial Function Scientific Update Sponsored by Endothelix Inc.www.endothelix.com
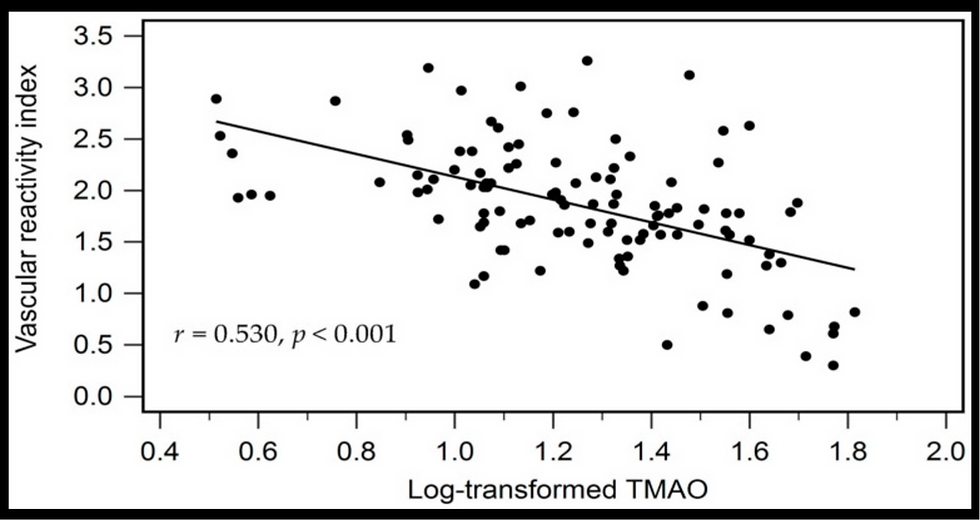
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments