What diet patients should get on after a heart attack? Low fat, low carb, low cal, or else?
- heartlung
- Jan 16, 2023
- 3 min read
Updated: Jan 18, 2023
New study shows you must listen to endothelial function.
Mediterranean diet and endothelial function in patients with coronary heart disease: An analysis of the CORDIOPREV randomized controlled trial
Elena M. Yubero-Serrano , Carolina Fernandez-Gandara , Antonio Garcia-Rios, Oriol A. Rangel-Zuñiga, Francisco M. Gutierrez-Mariscal, ose D. Torres-Peña, Carmen Marin, Javier Lopez-Moreno, Justo P. Castaño, Javier Delgado-Lista, Jose M. Ordovas, Pablo Perez-Martinez , Jose Lopez-Miranda
Unidad de Gestión Clinica de Medicina Interna, Lipids and Atherosclerosis Unit, Maimonides Institute for Biomedical Research in Córdoba, Reina Sofia University Hospital, University of Córdoba, Córdoba, Spain, CIBER Physiopathology of Obesity and Nutrition (CIBEROBN), Institute of Health Carlos III, Madrid, Spain
Abstract
Background
Endothelial dysfunction is a crucial step in atherosclerosis development, and its severity is determinant for the risk of cardiovascular recurrence. Diet may be an effective strategy to protect the endothelium, although there is no consensus about the best dietary model. The CORonary Diet Intervention with Olive oil and cardiovascular PREVention (CORDIOPREV) study is an ongoing prospective, randomized, single-blind, controlled trial in 1,002 coronary heart disease (CHD) patients, whose primary objective is to compare the effect of 2 healthy dietary patterns (low-fat versus Mediterranean diet) on the incidence of cardiovascular events. Here, we report the results of one secondary outcome of the CORDIOPREV study: to evaluate the effect of these diets on endothelial function, assessed by flow-mediated dilation (FMD) of the brachial artery.
Methods and findings
From the total participants taking part in the CORDIOPREV study, 805 completed endothelial function study at baseline and were randomized to follow a Mediterranean diet (35% fat, 22% monounsaturated fatty acids [MUFAs], and <50% carbohydrates) or a low-fat diet (28% fat, 12% MUFAs, and >55% carbohydrates), with endothelial function measurement repeated after 1 year. As secondary objectives and to explore different underlying mechanisms in the modulation of endothelial function, we quantified endothelial microparticles (EMPs) and endothelial progenitor cells (EPCs) and evaluated, in 24 preselected patients, in vitro cellular processes related to endothelial damage (reactive oxygen species, apoptosis, and senescence) and endothelial repair (cell proliferation and angiogenesis), as well as other modulators (micro-RNAs [miRNAs] and proteins). Patients who followed the Mediterranean diet had higher FMD (3.83%; 95% confidence interval [CI]: 2.91–4.23) compared with those in the low-fat diet (1.16%; 95% CI: 0.80 to 1.98) with a difference between diets of 2.63% (95% CI: 1.89–3.40, p = 0.011), even in those patients with severe endothelial dysfunction. We observed higher EPC levels (group difference: 1.64%; 95% CI: 0.79–2.13, p = 0.028) and lower EMPs (group difference: −755 EMPs/μl; 95% CI: −1,010 to −567, p = 0.015) after the Mediterranean diet compared with the low-fat diet in all patients. We also observed lower intracellular reactive oxygen species (ROS) production (group difference: 11.1; 95% CI: 2.5 to 19.6, p = 0.010), cellular apoptosis (group difference: −20.2; 95% CI: −26.7 to −5.11, p = 0.013) and senescence (18.0; 95% CI: 3.57 to 25.1, p = 0.031), and higher cellular proliferation (group difference: 11.3; 95% CI: 4.51 to 13.5, p = 0.011) and angiogenesis (total master segments length, group difference: 549; 95% CI: 110 to 670, p = 0.022) after the Mediterranean diet than the low-fat diet. Each dietary intervention was associated with distinct changes in the epigenetic and proteomic factors that modulate biological process associated with endothelial dysfunction. The evaluation of endothelial function is a substudy of the CORDIOPREV study. As in any substudy, these results should be treated with caution, such as the potential for false positives because of the exploratory nature of the analyses.
Conclusions
Our results suggest that the Mediterranean diet better modulates endothelial function compared with a low-fat diet and is associated with a better balance of vascular homeostasis in CHD patients, even in those with severe endothelial dysfunction.
Clinical trial registration:
URL, http://www.cordioprev.es/index.php/en. clinicaltrials.gov number NCT00924937.

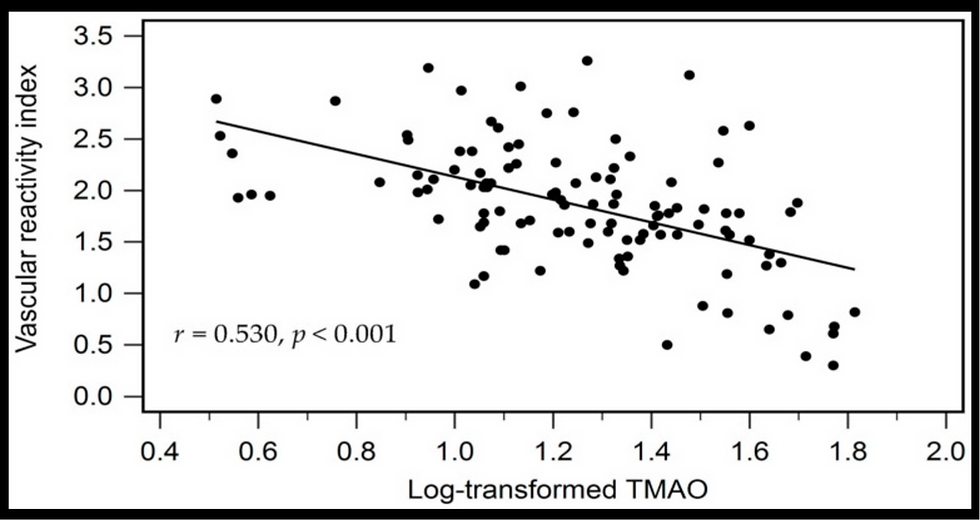
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments