Association of Endothelial Dysfunction With Chronic Marijuana Smoking and THC-Edible Use
- heartlung
- Sep 12
- 2 min read
JAMA Cardiol.2025 Aug 1;10(8):851-855.
Leila Mohammadi, Mina Navabzadeh, Nerea Jiménez-Téllez, Daniel D Han, Emma Reagan, Jordan Naughton, Lylybell Y Zhou , Rahul Almeida, Leslie M Castaneda, Shadi A Abdelaal, Kathryn S Park , Keith Uyemura, Christian P Cheung, Mehmet Nur Onder, Natasha Goyal, Poonam Rao, Judith Hellman, Jing Cheng, Joseph C Wu, Gregory M Marcus, Matthew L Springer
Abstract
Importance: Recreational and medicinal cannabis legalization has led to increased cannabis use. To understand the consequences for vascular health, we initiated the CANnabis: Does It Damage Endothelium (CANDIDE) study.
Objective: To investigate whether cannabis use is associated with vascular endothelial dysfunction.
Design, setting, and participants: In this cross-sectional study, age-matched healthy adults, aged 18 to 50 years, living in the San Francisco Bay Area, California, who neither smoke tobacco nor vape and were not frequently exposed to secondhand smoke were recruited into 3 cohorts: 2 chronic cannabis user groups (marijuana smokers and tetrahydrocannabinol [THC]-edible users) and 1 nonuser group. Participants were recruited from October 25, 2021, through August 1, 2024; analysis was completed September 2024. Participants' arterial flow-mediated dilation (FMD) and carotid-femoral pulse wave velocity (PWV) were measured. Human umbilical vein endothelial cells (HUVECs) were exposed to participant sera with and without vascular endothelial growth factor (VEGF) to assess the effects of user serum on endothelial nitric oxide production.
Main outcomes and measures: FMD and PWV were direct physiological measurements, and VEGF-stimulated nitric oxide production was measured from HUVECs incubated in user serum samples.
Results: Among 55 participants (20 female [37%]; 35 male [63%], mean age, 31.3 [SD, 8.4] years) arterial FMD was significantly lower among the marijuana smokers (mean, 6.0% [SD, 2.6%]; P = .004) and lower among THC-edible users (mean, 4.6% [SD, 3.7%]; P = .003) than among nonusers (mean, 10.4% [SD, 5.2%]). VEGF-stimulated nitric oxide levels in endothelial cells treated with participants' sera were significantly lower for the marijuana smoker group (mean, 1.1 nmol/L [SD, 0.3 nmol/L] ) than for the nonuser group (mean, 1.5 nmol/L [SD, 0.3 nmol/L]; P = .004) but were unaffected among the THC-edible users group compared with the nonusers (mean, 1.5 nmol/L [SD, 0.3 nmol/L]; P = .81). FMD was inversely correlated with smoking frequency (r = -0.7; P < .001) and the amount of THC ingested (r = -0.7; P = .03). Other vascular properties showed no differences.
Conclusions: This cross-sectional study found that chronic cannabis smoking and THC ingestion were associated with endothelial dysfunction similar to that observed in tobacco smokers, although apparently occurring via distinct mechanisms.

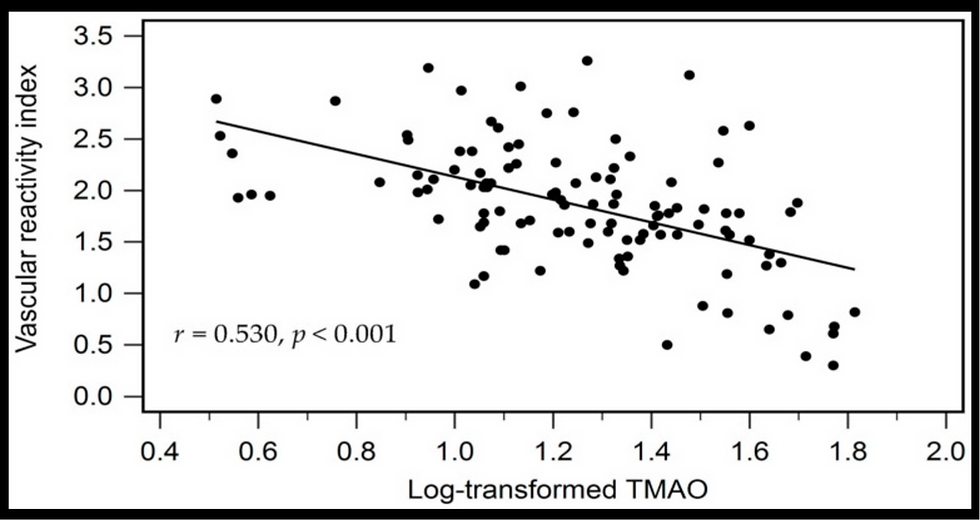
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments