Melatonin as a potential adjuvant treatment of COVID-19?
- heartlung
- Jan 16, 2023
- 4 min read
Rev Med Virol. 2020 Apr 21 Melatonin: Roles in influenza, Covid-19, and other viral infections. Anderson G1, Reiter RJ2. Author information 1 CRC Scotland & London, London, UK. 2 Department of Cellular and Structural Biology, University of Texas Health Science at San Antonio, San Antonio, Texas. Abstract There is a growing appreciation that the regulation of the melatonergic pathways, both pineal and systemic, may be an important aspect in how viruses drive the cellular changes that underpin their control of cellular function. We review the melatonergic pathway role in viral infections, emphasizing influenza and covid-19 infections. Viral, or preexistent, suppression of pineal melatonin disinhibits neutrophil attraction, thereby contributing to an initial “cytokine storm”, as well as the regulation of other immune cells. Melatonin induces the circadian gene, Bmal1, which disinhibits the pyruvate dehydrogenase complex (PDC), countering viral inhibition of Bmal1/PDC. PDC drives mitochondrial conversion of pyruvate to acetyl-coenzyme A (acetyl-CoA), thereby increasing the tricarboxylic acid cycle, oxidative phosphorylation, and ATP production. Pineal melatonin suppression attenuates this, preventing the circadian “resetting” of mitochondrial metabolism. This is especially relevant in immune cells, where shifting metabolism from glycolytic to oxidative phosphorylation, switches cells from reactive to quiescent phenotypes. Acetyl-CoA is a necessary cosubstrate for arylalkylamine N-acetyltransferase, providing an acetyl group to serotonin, and thereby initiating the melatonergic pathway. Consequently, pineal melatonin regulates mitochondrial melatonin and immune cell phenotype. Virus- and cytokine-storm-driven control of the pineal and mitochondrial melatonergic pathway therefore regulates immune responses. Virus-and cytokine storm-driven changes also increase gut permeability and dysbiosis, thereby suppressing levels of the short-chain fatty acid, butyrate, and increasing circulating lipopolysaccharide (LPS). The alterations in butyrate and LPS can promote viral replication and host symptom severity via impacts on the melatonergic pathway. Focussing on immune regulators has treatment implications for covid-19 and other viral infections. © 2020 John Wiley & Sons, Ltd. KEYWORDS: aryl hydrocarbon receptor; covid-19; immune; influenza; melatonin; metabolism; mitochondria; sirtuin; treatment; viral infection

COVID-19: Melatonin as a potential adjuvant treatment
Rui Zhang,a Xuebin Wang,a Leng Ni,a Xiao Di,a Baitao Ma,a Shuai Niu,a Changwei Liu,a,⁎ and Russel J. Reiterb,⁎⁎
⁎⁎Correspondence to: Russel J. Reiter, Cell Biology, Journal of Pineal Research, Melatonin Research, Thomson Reuters list of Highly Cited Scientists, Clarivate Analytics list of Highly Cited Scientists, Department of Cell Systems and Anatomy, UT Health San Antonio, San Antonio, TX 78229, USA reiter@uthscsa.edu
Abstract
This article summarizes the likely benefits of melatonin in the attenuation of COVID-19 based on its putative pathogenesis. The recent outbreak of COVID-19 has become a pandemic with tens of thousands of infected patients. Based on clinical features, pathology, the pathogenesis of acute respiratory disorder induced by either highly homogenous coronaviruses or other pathogens, the evidence suggests that excessive inflammation, oxidation, and an exaggerated immune response very likely contribute to COVID-19 pathology. This leads to a cytokine storm and subsequent progression to acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) and often death. Melatonin, a well-known anti-inflammatory and anti-oxidative molecule, is protective against ALI/ARDS caused by viral and other pathogens. Melatonin is effective in critical care patients by reducing vessel permeability, anxiety, sedation use, and improving sleeping quality, which might also be beneficial for better clinical outcomes for COVID-19 patients. Notably, melatonin has a high safety profile. There is significant data showing that melatonin limits virus-related diseases and would also likely be beneficial in COVID-19 patients. Additional experiments and clinical studies are required to confirm this speculation.
Keywords: COVID-19, SARS-CoV-2, Melatonin, Oxidation-reduction, Cytokines, Immunomodulation

Life Sci. 2020 Apr 22:117716. Correspondence COVID-19: Melatonin as a potential adjuvant treatment. Salles C1. would like to congratulate you for the published article “COVID-19: Melatonin as a potential adjuvant treatment “1 and, at the same time, I would like to make some complementary considerations regarding COVID-19, melatonin, sleep deprivation and lung tissue. We know that during sleep there is production of pro-and anti-inflammatory cytokines, however, production of inflammatory cytokines is observed in sleep deprivation. In the experimental study by Nunes et al2, it was possible to demonstrate that mice in sleep deprivation had more inflammatory cytokines than those allowed for good quality sleep. In addition, mice in sleep deprivation after corticotherapy (dexamethosone) were not able to reduce production of IL-17 and TNF- alpha in the same way as mice that had good quality of sleep. Thus, this study shows that sleep deprivation aggravated the inflammatory process in lung tissue, and limited the action of corticotherapy. Given this scenario, I pose the following question: Is sleep deprivation able to negatively interfere with the lung picture of COVID-19? On the other hand, it is known that mortality incidence of COVID-19 is much higher in the elderly, a population that frequently presents complaints both to initiate and to maintain sleep, and that melatonin, when well indicated, has a good response, increasing hours of sleep. Thus, I would like to suggest an investigation of sleep deprivation to patients with COVID-19, and ask a second question: Would the use of melatonin, especially in elderly patients in sleep deprivation with COVID-19, in an early and even preventive way, be able to reduce the injury in the lung tissue of these patients? Finally, I congratulate Zhang et al. for the research conducted, as well as my respect to the considerations exposed regarding COVID-19 and melatonin.
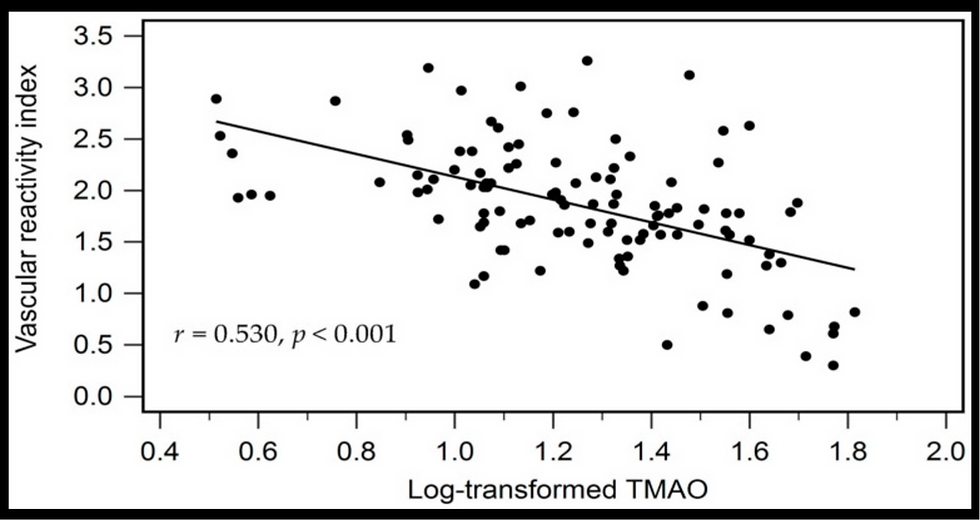
![Lipoprotein(a) levels predict endothelial dysfunction in maintenance hemodialysis patients: evidence from [VENDYS] vascular reactivity index assessment](https://static.wixstatic.com/media/dac531_5285607cc591409a9d83746f042af7c6~mv2.png/v1/fill/w_980,h_980,al_c,q_90,usm_0.66_1.00_0.01,enc_avif,quality_auto/dac531_5285607cc591409a9d83746f042af7c6~mv2.png)

Comments